Obstructive Sleep Apnea (OSA)
Sleep apnea is a sleep disorder that causes you to stop breathing during your sleep. It is when you stop breathing for 10 seconds or more, something that can happen at least five times an hour, while you sleep.

- Loud, chronic snoring
- Bed partner reporting breathing interruptions
- Gasping or choking during sleep
- Restless sleep
- Morning headaches
- Daytime sleepiness
Millions of people suffer from sleep apnea. And yet, most of them are not aware of it.
There are three types of sleep apnea.
Obstructive sleep apnea (OSA) – this is when your upper airways become blocked while you sleep, thereby reducing or completely stopping airflow.
Central sleep apnea (CSA) – it occurs when your brain does not send the signals needed to breathe.
Complex sleep apnea (also called mixed sleep apnea) – a combination of obstructive sleep apnea and central sleep apnea.
PIE CHART GOES HERE
What is it?
Obstructive sleep apnea is the most common type of sleep apnea.
It is a condition characterized by recurring episodes of partial or complete obstruction of the respiratory airways during sleep.
Airway obstructions may be described as hypopneas or apneas:
- If airflow is reduced by 90% or more for at least 10 seconds, it is described as an apnea.
- If airflow is reduced by at least 30% for 10 seconds or more, the episode may be called a hypopnea.
![]()
The number of episodes of partial and complete airway obstructions can help doctors determine the severity of OSA.
The severity of sleep apnea is usually measured using the apnea-hypopnea index (AHI), i.e. the mean number of apneas and hypopneas per hour of sleep.
There are different levels of sleep apnea severity:
- Mild sleep apnea: An AHI of five to 14 events per hour
- Moderate sleep apnea: An AHI of 15 to 29 events per hour
- Severe sleep apnea: An AHI of 30 or more events per hour
![]()
In all cases, sleep apnea can affect a person’s quality of life. It is also a risk factor for many potentially lethal illnesses.
You may also find that your doctor refers you to the Epworth Sleepiness Scale. Originally introduced in 1991 by Dr Murray Johns of Epworth Hospital in Melbourne, Australia, a short questionnaire is used to diagnose sleep disorders and measure daytime sleepiness levels.
What happens during obstructive sleep apnea?
Obstructive sleep apnea usually occurs when the muscles that control the airways relax too much while you are sleeping, thereby causing the throat to narrow.
This is what happens:
- Your tongue drops onto the soft tissue to be found on the roof of your mouth, thus pushing it against the back of the throat. The upper airway then gets partially or completely blocked.
- When this happens, the brain sends an alarm to open the airway. This is most often associated with a brief awakening from sleep. During that brief moment, the brain quickly reactivates the muscles that hold the throat open, letting air through to restore oxygen levels. The brain then goes back to sleep. This awakening is usually so brief that you don't remember it.
This cycle can repeat hundreds of times each night, and cause abnormal levels of both oxygen and carbon dioxide in the blood, as well as fragmented sleep. All of this leads to severe health consequences if left untreated.
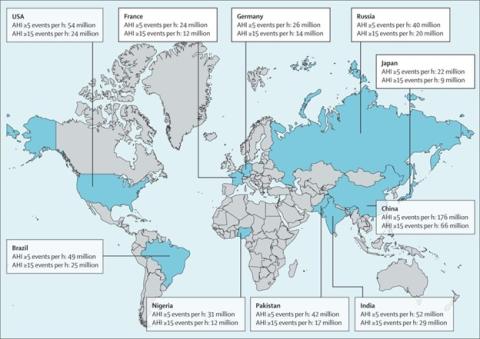
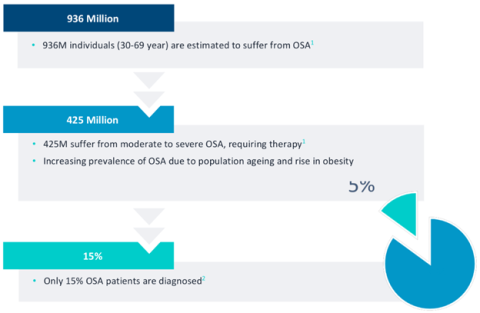
How common is obstructive sleep apnea?
Most people don't know they have sleep apnea.
Obstructive sleep apnea is a common sleep disorder.
A recent analysis published in The Lancet suggests that more than 930 million adults aged 30–69 years may suffer from obstructive sleep apnea worldwide.
How do I know if I suffer from obstructive sleep apnea?
People with obstructive sleep apnea might not be aware of their interrupted sleep.
Some signs of obstructive sleep apnea are:
- Bed partner may report loud, disruptive snoring or hearing a sleeper gasp, choke, snort, or stop breathing during sleep.
- Morning symptoms: Waking up with a headache, dry mouth, or the need to urinate may be signs of underlying obstructive sleep apnea. Morning headaches may last for hours and occur most days.
- Feeling excessively tired during the day: obstructive sleep apnea is the most common medical cause of excessive daytime sleepiness. People with OSA may fall asleep during monotonous activities, like reading or watching TV, and may try to combat persistent sleepiness with caffeine.
Think you may have sleep apnea? It’s important to have it checked.
Typical symptoms?
- Loud snoring
- A dry mouth when you waken
- Headache in the morning
- Difficulty staying asleep – this is known as insomnia
- Excessive daytime drowsiness – this is known as hypersomnia
- Difficulty paying attention when awake
- Times when you stop breathing during sleep, as reported by another person
And yet, even though obstructive sleep apnea is common, cases often go undiagnosed. Indeed many people may not even be aware that they are experiencing these symptoms, so they continue living undiagnosed and untreated.
<< Block
Help us spread the word about obstructive sleep apnea.
[Share buttons]
>>
What are the main risk factors?
Anyone can develop obstructive sleep apnea, though certain factors put you at increased risk:
- Age: Sleep apnea can occur at any age, but the risk increases as you get older. This is because fatty tissue can build up in your neck and the tongue as you age, thereby raising the risk of sleep apnea.
- Body mass index (BMI): The likelihood of developing OSA goes up with a person’s BMI, a measure of body fat based on a person’s height and weight. Overweight people can have increased fat deposits in their necks, which can block the upper airway.
Certain physical features also make a person more likely to develop OSA. These include:
- A small or set-back lower jaw.
- Large tonsils and a thick neck. These features may cause sleep apnea because they narrow the upper airway.
- Large tongue: a large tongue in the mouth can block the airway while sleeping.
- Excess fat surrounding the throat.
- Endocrine disorders, or changes in your hormone levels. Hormone levels can affect the size and shape of your face, tongue, and airway. People who have low levels of thyroid hormones or high levels of insulin or growth hormone have a higher risk of sleep apnea.
Other risk factors may include:
- Family background and genetics. Sleep apnea can be inherited, as genes determine the size and shape of your skull, face, and upper airway. Additionally, your genes may increase the risk of other health conditions that may lead to sleep apnea.
- Lifestyle habits: Drinking alcohol and smoking can raise the risk of sleep apnea. Alcohol can make the muscles of the mouth and throat relax, leading to closure of the upper airway. Smoking can also cause inflammation in your upper airway, which affects breathing.
- Nasal congestion: A stuffy nose may double a person’s chances of experiencing OSA. Nasal congestion can be caused by a variety of factors, including colds, sinus infections, and/or the flu.
How is Obstructive Sleep Apnea Diagnosed?
Sleep apnea is a serious medical problem that is both underdiagnosed and under-treated.
To diagnose obstructive sleep apnea, doctors look at a patient’s medical history and symptoms, conduct a physical exam, and refer them for a sleep study.
Medical history
While reviewing a person’s medical history, a doctor may inquire about risk factors as well as both nighttime and daytime symptoms. In some cases, a doctor may have a person fill out a questionnaire to look for additional symptoms and help differentiate between OSA and other conditions.
As sleepers may not recognize their night-time symptoms, roommates, bed partners and relatives may be asked to report a person's symptoms.
Physical Exam
Doctors typically perform a physical examination to check for physical features that increase the risk of OSA, including a person’s neck and waist size, and signs of health complications associated with OSA.
Sleep study
A sleep study is necessary to confirm (or repudiate) a diagnosis of obstructive sleep apnea, and also measure the severity of breathing disruptions. Also called polysomnography, a sleep study involves an overnight stay at a specialized sleep laboratory, often located within a sleep center or hospital.
Sometimes a sleep study can be completed at home with a portable sleep monitor.
When considered together with a person’s symptoms, the number of breathing events per hour found during a sleep study can help doctors determine the severity of OSA.
Obstructive sleep apnea treatment
Treatment of complex sleep apnea syndrome may involve a combination of interventions, including treatment of any underlying conditions and the use of continuous positive airway pressure (CPAP) or other modes of positive airway pressure.
People suffering from OSA should discuss their symptoms with a sleep doctor to find the most effective treatment for them, as patients are quite different and require tailored approaches.
Positive airway pressure (PAP)
The primary treatment for OSA is positive airway pressure (PAP) therapy.
PAP therapy involves the use of pressurized air that is pumped through a bedside machine and into the nose and/or mouth of the patient to keep the airway open during sleep.
<< Include some pictures of patients sleeping with CPAP >>
PAP therapy may be provided using one of the following methods:
- continuous positive airway pressure (CPAP)
- bilevel positive airway pressure (BiPAP or BPAP)
- auto-titrating positive airway pressure (APAP)
Although CPAP has proven to be a very effective treatment for obstructive sleep apnea, patients are often uncomfortable with the device and adherence to this type of treatment remains problematic. For this reason, alternative sleep apnea treatments have been developed in recent years.
Hypoglossal nerve stimulation, a proven alternative to CPAP therapy
Thousands of patients worldwide rely on hypoglossal nerve stimulation to treat their obstructive sleep apnea.
In recent years, new and innovative treatments have emerged for patients who do not tolerate PAP therapy. One of the most promising angles is hypoglossal nerve stimulation.
Hypoglossal nerve stimulation (HGNS) is an alternative treatment for obstructive sleep apnea that electrically stimulates the nerves of the tongue – the hypoglossal nerve that enables tongue movement – to prevent upper airway obstruction.
Hypoglossal nerve stimulation is a serious option for people looking for an alternative to CPAP therapy. The effectiveness of this treatment has been scientifically proven.
Hypoglossal nerve stimulation helps to prevent the potential side effects of CPAP therapy such as dry mouth, nasal congestion or skin irritation caused by the mask.
As it does not involve a CPAP device, it doesn’t make noise and is really discreet.
Surgery
Surgery is for people who have extra or uneven tissue that blocks airflow through the nose or throat. For example, if you have a deviated nasal septum, swollen tonsils, and adenoids, or a small lower jaw that causes your throat to be too narrow, surgery might help you.
Surgery remains a last resort option. Doctors usually try other treatments first.
Oral devices / Mandibular advancement devices (MAD)
Dental appliances or oral "mandibular advancement" devices keep your tongue from blocking your throat or bring your lower jaw forward. This may help keep your airway open while you sleep.
MAD therapy is usually more suitable for mild to moderate obstructive sleep apnea.
Behavior changes
Behavior and lifestyle changes can also be a starting point in the treatment of OSA as it allows most people to better manage their condition:
- Weight loss can be an answer. Even losing 10% of your weight could make a difference.
- Alcohol and/or sleeping pills should be avoided, as these tend to close the airway during sleep keeping you from breathing like you should for longer periods.
- Sleeping on your side can help if you get mild sleep apnea when sleeping on your back.
- Nasal sprays can help if sinus problems or nasal congestion make it harder to breathe while you sleep.
Risks & complications of untreated OSA
When the quality of your sleep is compromised, your body isn’t able to repair itself.
Untreated obstructive sleep apnea is associated with numerous negative health consequences:
- Drowsy driving: Driving accidents are a significant risk for people with OSA. In fact, people with OSA are two to three times more likely to be involved in a car accident than people without OSA.
- Mental health changes: OSA is associated with a variety of mental health changes, including irritability, depression, and anxiety. People with OSA may also experience impaired attention, memory, and an increased risk of making errors.
- Cardiovascular disease: OSA increases the risk of health conditions affecting the heart and blood vessels, such as hypertension, an irregular heartbeat, and heart failure. OSA also increases the risk of stroke.
- Diabetes: People with OSA have a higher likelihood of being resistant to insulin, metabolic syndrome, and type 2 diabetes. OSA can also increase the likelihood of developing complications from diabetes.
![]()
Untreated OSA can be deadly:
- 2 times increase risk of stroke
- 2.5 times increased risk of heart failure
- 5 times more risk of cardiovascular mortality
Living with Sleep Apnea
It’s important for people who are diagnosed with obstructive sleep apnea to be well informed about their diagnosis, and understand the importance of appropriate treatment. While OSA typically cannot be cured, treatment does help most people reduce breathing disruptions, improve sleep quality, and minimize health consequences.
The following tips can help people learn to live with OSA:
- Find support: Daily use of PAP therapy or other treatments can be a significant adjustment for people diagnosed with OSA. Connecting with other people with OSA through websites and support groups may be a helpful first step in locating accurate information and social support.
- Be cautious when driving. The side effects of OSA can make it difficult to concentrate and stay alert. People with OSA should be aware of the risks of driving, operating machinery, and performing other dangerous tasks.
- Follow up regularly with a doctor. After a diagnosis of OSA, people should maintain frequent communication with a doctor or sleep specialist to ensure that their treatment is working. Side effects should be monitored over time.
- Avoid substances that worsen OSA. For people living with OSA, it’s important to avoid substances that could aggravate breathing issues during sleep. Be sure to talk to a doctor before using sedatives, muscle relaxants, benzodiazepines, narcotics, and alcohol.
- Talk to your doctors about OSA. To prevent airway obstructions, people with OSA need special care when receiving anesthesia or pain medications. As a result, people should discuss their diagnosis with all their doctors and medical professionals.
Do you still feel tired when you wake up?
People living with sleep apnea should also ensure that they get enough sleep each night. In addition to following their prescribed treatment plan, people can improve their sleep by following basic sleep hygiene practices:
- Avoid caffeine late in the day, including soda, tea, and chocolate.
- Don’t drink alcohol at night.
- Quit smoking altogether, or at a minimum avoid smoking in the evenings.
- Exercise regularly.
- Limit any noises in the bedroom.
- Keep the bedroom as dark and comfortable as possible.
Sleep apnea glossary
Apnea
Sleep apnea is when you stop breathing for 10 seconds or more while you’re asleep. If airflow is reduced by 90% or more for at least 10 seconds, it is described as an apnea.
Hypopnea
Hypopnea is overly shallow breathing or an abnormally low respiratory rate.
Hypopnea is typically defined via a decreased amount of air movement into the lungs and may cause oxygen levels in the blood to drop. It is commonly due to partial obstruction of the upper airway.
Hypopnea is a partial loss of breath for 10 seconds or longer.
If airflow is reduced by at least 30% for 10 seconds or more, the episode may be called a hypopnea.
Apnea-Hypopnea Index (AHI)
Apnea-Hypopnea Index measures sleep apnea severity. The AHI is the sum of the number of apneas (pauses in breathing) plus the number of hypopneas (periods of shallow breathing) that occur, on average, each hour.
Working in collaboration with Dr. William C. Dement, Dr. Guilleminault established the apnea–hypopnea index to characterize the presence and severity of sleep apnea.
- AHI = sum of the number of apneas (pauses in breathing) plus the number of hypopneas (periods of shallow breathing) occurring, on average, each hour.
- Apneas and hypopneas must last at least 10 seconds to be called events.
- The Apnea-Hypopnea Index is calculated by dividing the number of events by the number of hours of sleep.
AHI is used to characterize the presence and severity of sleep apnea as well as to evaluate treatment outcome.
There are 4 levels of AHI for sleep apnea patients:
- Normal sleep: An AHI of fewer than five events, on average, per hour
- Mild sleep apnea: An AHI of five to 14 events per hour
- Moderate sleep apnea: An AHI of 15 to 29 events per hour
- Severe sleep apnea: An AHI of 30 or more events per hour
![]()
Mild obstructive sleep apnea
Mild obstructive sleep apnea is a grade of severity of sleep apnea corresponding to 5 to 14 apnea or hypopnea events per hour of sleep (AHI >= 5 and <= 14).
Moderate obstructive sleep apnea
Moderate obstructive sleep apnea is a grade of severity of sleep apnea corresponding to 15 to 29 apnea or hypopnea events per hour of sleep (AHI >= 15 and <= 29).
Severe obstructive sleep apnea
Severe obstructive sleep apnea is a grade of severity of sleep apnea corresponding to 30 or more apnea or hypopnea events per hour of sleep (AHI >= 30).
References
- https://www.webmd.com/sleep-disorders/sleep-apnea/understanding-obstruc…
- https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/…
- http://acronymsandslang.com/definition/903924/OSAS-meaning.html
- https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/…
- https://www.sleepfoundation.org/sleep-apnea/obstructive-sleep-apnea
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4561280/
- https://jcsm.aasm.org/doi/10.5664/jcsm.6034
- https://en.wikipedia.org/wiki/Sleep_apnea#Classification
- https://www.aastweb.org/blog/obstructive-vs.-central-sleep-apnea-key-di…;
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3917481/
- https://www.aastweb.org/blog/scoring-obstructive-hypopnea-vs-central-hy…
- https://www.sleepapnea.org/what-does-ahi-represent/
- https://www.sciencedirect.com/science/article/abs/pii/S1087079216300648…;
- https://psychcentral.com/health/why-psychologists-are-starting-to-care-…;
- https://www.nhlbi.nih.gov/health/sleep-apnea
- https://www.mayoclinic.org/diseases-conditions/obstructive-sleep-apnea/…;
- https://pubmed.ncbi.nlm.nih.gov/21652236/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6949509/